Did you read the previous part about Diaper Rash?
Atopic dermatitis (eczema) is the most common chronic inflammatory skin illness. Eczema can start at two or three months of age. It affects 10-30% of children (1:5/6 children) and is often associated with other atopic disorders such as asthma and seasonal allergies. When talking about atopic dermatitis, we often refer to the notion of atopic march, which explains that poor control of skin at a young age can lead to the risk of developing asthma and seasonal allergies later in life. This means that controlling eczema early in life is essential to prevent other medium and long-term conditions.
The cause of atopic eczema is above all genetic and involves a breakdown of the cutaneous barrier, often with the mutation of a gene called filaggrin. In layman’s terms, the skin as trouble maintaining water, which leads to significant drying of the cutaneous barrier. This leads to skin breakdown, which activates the body’s immune system to protect it from pathogenic agents in the environment. The body’s protective response leads to increased blood circulation and an immune system reaction that can lead to a yellowish discharge and the formation of yellowish crust. Healthy skin bacteria are activated, which can lead to local infections. A child that develops atopic eczema at a young age (usually in the first two years) has about a 60% chance of it being resolved after 12 years of age.
Infant eczema (<2 years) develops after two months of life and usually starts with the cheeks. Small red patches on the cheeks can become crusty and damp. Then the head, neck and arm extensors can be affected. The diaper zone is usually free of patches because of its damp environment.
After two years of age, the eczema patches are mostly found in elbow and knee folds. Other zones can also be affected (around the mouth, neck and wrists/ankles).
Atopic eczema is associated with severe itching and scratching which can worsen the condition.
Explanations:
- Eczema is caused by a breakdown in the skin’s cutaneous barrier, making it more permeable, and more likely to react to irritant substances in the environment (hypersensitivity). Following the skin’s reaction to the environment, the immune system reactions, leading to cutaneous inflammation.
- Eczema patches can appear between the ages of three months and two years, but very rarely after five.
- At least one child in six will be diagnosed with eczema.
- Eczema changes over time, with outbreaks and episodes.
- Over the years, there may be a general drying of the skin.
- As a general rule, eczema is not associated with food. Sometimes the patches and itching may increase when a child eats acidic foods, such as tomatoes or strawberries, but this is not a food allergy.
Recommendations:
- Some studies show that breastfeeding for as long as possible can help prevent eczema in a baby with genetic predispositions.
- Give your baby a 10 minute (maximum) warm bath once a day. This can help hydrate their skin. Make sure that they aren’t overly dried after. Pat them dry and then HYDRATE, HYDRATE and HYDRATE SOME MORE with a very hydrating cream, even if the baby doesn’t have red patches. Baths remove bacteria that can be found on the skin and lead to an infection, red patches and superinfection over the long run. HYDRATION is the FOUNDATIONAL TREATMENT. Prevention is as well.
- Use fragrance-free soap or cleansing oil to hydrate their skin (ex.: Uriage cleansing oil, Cutibase cleansing cream, Exomega cleansing oil, Derma smooth).
- The soap you use for your baby’s clothes should be mild and fragrance-free (ex.: Tide Zero) and don’t use a fabric softener.
- Softly dry your baby after the bath, patting, not rubbing, their skin.
- Apply an ultra-hydrating cream on the baby’s whole body. This cream must be fragrance-free and should be applied several times a day for babies with very dry skin (Uriage Bariéderm, Cutibase, Cerave, Aquaphor, Glaxal-Base, Aveeno Sensitive, Lipikart AP+, Exomega, Arbonne for Babies, Mustela Stelatopia Cream and Dermakalm are examples).
- Loose clothing is more appropriate for your baby, made out of cotton or soft materials. Wool and synthetic materials should not be used. Ideally, use cotton sheets.
- Itching is possible, so you should cut your baby’s nails to prevent scratches. You can also have them wear mittens during the day if the situation calls for it.
- To soothe their itching, you can spray the areas with mineral water. For extensive eczema, you will often have to use an anti-itch product, such as Atarax (prescription). This is very important if the baby is very bothered by the itching, as they will scratch it and break the skin, so back to the starting point! A vicious circle!
- Learn to recognise and avoid things that seem to cause outbreaks by your child.
- Consult a doctor for appropriate treatment if the situation doesn’t improve. Suitable corticosteroid cream is often necessary to control and treat their eczema, and it’s not dangerous for your baby’s skin. There are other treatment options, based on each child. You can use Betaderm, Protopic and many other products. Some creams don’t include cortisone but can be combined with other products to control the sores. There are medicated powders that can be mixed with a hydrating cream to treat your child.
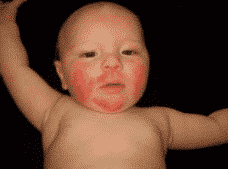


Photo source: aad.org, medecinenet.com, aaaai.org
To learn more, read my article Eczema and Babies.
Sources des photos : aad.org, medecinenet.com, aaaai.org

After reading this article, I am sure you have learned more about situations where your baby’s delicate skin can be irritated or worse. With the help of Dr. Bourgeault, you now better understand why these things happen and how to better react to the symptoms using practical advice.
Thanks to our expert for her help.
Talk soon,
Marie
The Baby Expert
Collaborator
Dr Bourgeault