It is true that urinary tract infections can be more common during pregnancy, and it is important to understand this phenomenon, as it is not without risk for an expectant mother and her baby.
This post aims to answer questions many pregnant women have about the occurrence of urinary tract infections during pregnancy.
Definition
A urinary tract infection is a disease caused by microbes, usually bacteria, that affect the urinary tract.
The urinary system of a human has a set of structures, namely:
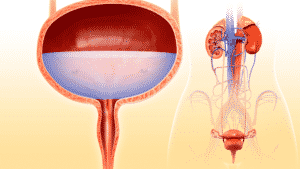 1- the urethra which designates the canal going from the urinary meatus to the bladder,
1- the urethra which designates the canal going from the urinary meatus to the bladder,
2- the bladder, which is a reservoir where urine is stored,
3- the ureter which corresponds to the canal going from the bladder to each kidney
4- The kidneys are responsible for filtering all the blood and are responsible for removing as many impurities as possible and eliminating them through urine.
When the infection is located in the lower part of the urinary system, namely the bladder, this inflammation is more specifically called “cystitis” which occurs in 1 to 4% of pregnant women.
In cases where the infection affects the kidneys, the upper part of the urinary system, it is more commonly referred to as pyelonephritis and its incidence is between 1 and 2%.
Bacteria involved
Escherichia coli (E. coli) is responsible for 90% of urinary tract infections in pregnant women, and group B streptococcus is responsible for about 5% of cases. These bacteria naturally live in the intestines of all people.
Factors that promote urinary tract infections during pregnancy
There are several factors that can predispose a pregnant woman to developing one or more urinary tract infections.
First, simply being a woman automatically puts us at a higher risk of developing a urinary tract infection due to our anatomy. A woman’s urinary meatus is much closer to the rectum and potential bacteria compared to men’s.
Several other reasons more attributable to pregnancy can also play a role in the onset of urinary tract infection symptoms. Here are some examples:
 1- The developing uterus will tend to put pressure on the urinary system, especially on the right side, due to the rotation of the growing uterus. This can slow down circulation in the urinary system and cause less waste to be evacuated.
1- The developing uterus will tend to put pressure on the urinary system, especially on the right side, due to the rotation of the growing uterus. This can slow down circulation in the urinary system and cause less waste to be evacuated.
2-Hormonal changes during pregnancy lead to physiological dilation of the urinary vessels, starting in the first trimester. The urinary meatus becomes more distended, opening the door to the spread of microbes from the outside. This relaxation also causes a possible reflux of urine from the bladder to the kidneys.
3-The relaxing effect of progesterone on the muscles will cause the bladder to dilate further and it will be more difficult to empty it completely when urinating, therefore, a bigger accumulation of waste.
4- With the displacement of the uterus, the bladder eventually ends up more in the abdominal cavity rather than inside the pelvis (pelvic level), which can cause pain when urinating. The position of the uterus pushes the bladder and can interfere with its functions.
5- Hormonal changes lead to an increase in the pH of urine. Urine is therefore less acidic, which has the consequence of reducing the antibacterial protection to fight microorganisms coming from outside.
6- The fact that the pregnant woman has a natural decrease in her physiological immune system, especially in the last trimester, can promote the invasion of bacteria in the urinary tract.
7- Being known as a woman who is predisposed to repeated urinary tract infections even before becoming pregnant.
8- Failure to urinate after sexual intercourse.
Detecting a urinary tract infection during pregnancy monitoring
In Canada, the most recent scientific evidence does not show a clear benefit of routine screening for urinary tract infections at every pregnancy follow-up visit. However, urine analysis and culture are an integral part of the recommended screening tests for all pregnant women during the first trimester.
Pregnant women who will need more monitoring, screening, and possibly treatment are pregnant women:
1- who have a significant history of recurrent urinary tract infections, that is, when they occur more than twice in 6 months or more than 3 times per year.
 2- who have a health condition such as diabetes, which can predispose these women to suffer more from recurrent urinary tract infections since the amount of sugar in their urine may be higher, which bacteria like.
2- who have a health condition such as diabetes, which can predispose these women to suffer more from recurrent urinary tract infections since the amount of sugar in their urine may be higher, which bacteria like.
3- who verbalize uncomfortable symptoms attributable to a urinary tract infection.
Some doctors still continue to perform the small strip test in the urine (urinary labstix) during certain follow-up visits to quickly analyze and detect whether or not there is a urinary infection, even if no symptoms are manifested (asymptomatic) by the expectant mother.
Symptoms:
Between 2 and 15% of pregnant women will unknowingly develop a urinary tract infection during their pregnancy, as they will not experience any particular symptoms. This situation can unfortunately develop into a full-blown infection, either cystitis or pyelonephritis.
If there are symptoms, they can appear suddenly or gradually, alone or in multiple forms.
- Burning sensation and pain when urinating
- More frequent and urgent urge to urinate without being able to (or only a few drops)
- Increased frequency of urination (pollakiuria)
- Urine is often darker, cloudy, or blurred
- Sometimes blood is present in the urine
- Sensation of pressure in the lower abdomen
- Sometimes, a strong odor may come from the urine.
Complications and prevention of urinary tract infections
Possible complications:
 When a urinary tract infection is not detected and treated early, it can progress to the upper part of the urinary system and cause a kidney infection (pregnancy pyelonephritis) in 20 to 40% of cases. In addition to fever, the pain of pyelonephritis is very intense and localized more specifically to the lumbar region of the back. Chills, nausea, and vomiting may also accompany this more specific infection.
When a urinary tract infection is not detected and treated early, it can progress to the upper part of the urinary system and cause a kidney infection (pregnancy pyelonephritis) in 20 to 40% of cases. In addition to fever, the pain of pyelonephritis is very intense and localized more specifically to the lumbar region of the back. Chills, nausea, and vomiting may also accompany this more specific infection.
Other possible complications include increased preterm labor, premature rupture of membranes, and growth retardation in in-utero babies.
Therefore, it is imperative that the pregnant woman describes to the health professional monitoring the pregnancy all her observations that could lead to the prevention of a urinary tract infection and its potential complications.
Prevention of urinary tract infections
To prevent a urinary tract infection, it goes without saying that basic hygiene measures are recommended and other initiatives can also be put forward to help the system better defend itself at the genitourinary level:
- Wash the genital area daily,
- Wipe or wash the genital area from front to back (without going back),
- Urinate before and after sexual intercourse,
- Avoid bubble baths and douching, which can limit the body’s natural defenses by reducing good protective bacteria,
- Eat a healthy diet, which helps support the immune system and maintain a slightly more acidic genitourinary pH balance,
- Drink water: up to 2 liters per day (equivalent to 8 glasses of water per day),
- Limit your consumption of coffee or spices, which can cause bladder irritation over time,
- Take probiotics,
- Some literature suggests drinking cranberry juice for its antibacterial properties that prevent cranberries from attaching to the urinary tract walls and causing infections,
Treatment of urinary tract infections
Any urinary tract infection diagnosed in a pregnant woman must be treated, even if the expectant mother has no particular symptoms. The goal is always to prevent potential complications for her and her baby.
It’s sure that pregnant women are advised to drink more water every day in order to eliminate as much bacteria as possible from their urinary system and better prevent the infection from spreading to their kidneys.
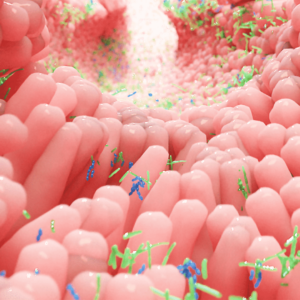 Several antibiotics can be safely prescribed during pregnancy. However, the effect of antibiotics on vaginal and intestinal flora is well known. Unfortunately, antibiotics attack not only bad bacteria, but also good ones, making it more vulnerable to vaginitis or vaginosis (french only). To counteract these effects, it is possible that taking probiotics would be beneficial to maintain the genitourinary environment as balanced as possible, always with a preventive approach.
Several antibiotics can be safely prescribed during pregnancy. However, the effect of antibiotics on vaginal and intestinal flora is well known. Unfortunately, antibiotics attack not only bad bacteria, but also good ones, making it more vulnerable to vaginitis or vaginosis (french only). To counteract these effects, it is possible that taking probiotics would be beneficial to maintain the genitourinary environment as balanced as possible, always with a preventive approach.
For more details on taking probiotics during pregnancy or while breastfeeding (french only).
Following drug treatment, you should expect to have one or more urine tests after the end of antibiotic therapy to ensure that the urinary tract infection has indeed resolved.
We hope that all this information will help you better understand urinary tract infections and their repercussions, better identify their symptoms and better prevent them.
Marie Fortier
The baby expert
To continue reading on the subject, see the articles: